

It happens not only in the arteries around the heart. Peripheral plaque is the kind of plaque in the arteries in the legs and feet.Īs I mentioned earlier, plaque is not localized. “Peripheral” refers to the outside of the heart area. If we can have it in one spot, then we can have it everywhere.
However, plaque doesn’t happen in a single artery. Plaque is the major cause of heart attack, stroke, Alzheimer’s disease, and other chronic conditions. That’s not surprising, as mostly the focus in medical practice is to measure the plaques in such locations. The price, though, is expensive.Īll the above tests attempt to look at plaque in the arteries of the heart. There have been some excellent studies (like SCOT-HEART & PROMISE) that prove the power of this technique. But it’s not 100% good-it doesn’t quantify very well, and it uses radiation.
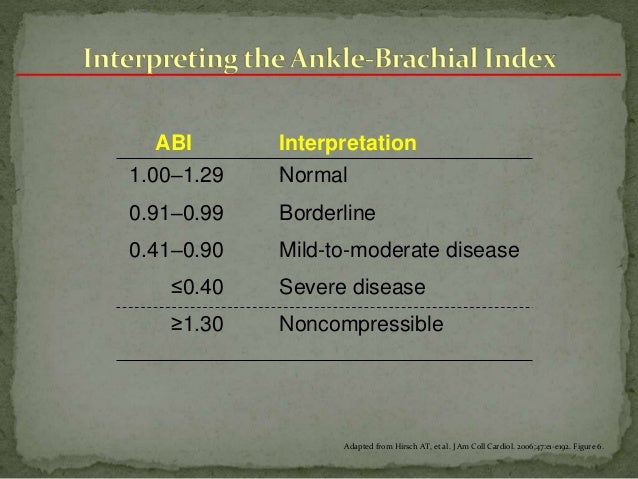
About a million people per year are tested this way, but it’s never going to be a great screening tool for an asymptomatic 30-year-old. You have to have over 50% occlusion to detect plaque. There’s the stress test that is used 5 million times a year. Aggressive treatment of this cohort with anticoagulants might be beneficial.It’s important to screen and measure coronary plaque. Interestingly, NC vessel patients compared to PAD patients had a statistically significant risk of a VTE event (adjusted HR: 1.24, 95% CI: 1.15-1.33, p-value< 0.001).Ĭonclusions: Compared to patients without PAD those with poorly compressible calcified lower extremity arteries are more prone to develop venous thromboembolic disease. However, patients with NC vessels had a statistically significant risk of developing VTE compared to patients with normal ABI (adjusted HR: 1.21, 95% CI: 1.12-1.30, p-value< 0.001). Compared to those without PAD, low ABI patients did not have a significantly increased risk of VTE (adjusted HR: 1.06, 95% CI: 1.00-1.11, p=0.04). Compared to normal ABI, patients with abnormal ABI were more likely to be older and male. Results: There were 38,016 unique patients (mean age 66.1 ± 14.8 years, female 42.3%) who underwent ABI measurement. Multivariate Cox proportional regression was used to calculate hazard ratios (HR) with 95% confidence intervals after adjusting for age, gender, and prior history of cancer, or incidence of VTE. The main outcome analyzed was new venous thromboembolism. Based on the ankle brachial index (ABI) recordings, patients were classified into 3 categories: patients with PAD (ABI1.4), and patients with normal ABI (1.0-1.4). Methods: We reviewed vascular studies between 1996 and August 2018. Patients with PAD are at increased risk for vascular complications however, there is little evidence for its association with thrombosis.Īims: To understand the relationship between arterial occlusive disease and venous thrombosis. PAD is associated with endothelial dysfunction and inflammation and shares several common risk factors with venous thrombosis. Theme: Arterial Thromboembolism » Peripheral Artery Diseaseīackground: Peripheral artery disease (PAD) impacts millions of people around the globe and is commonly diagnosed using lower extremity physiologic studies.


 0 kommentar(er)
0 kommentar(er)
